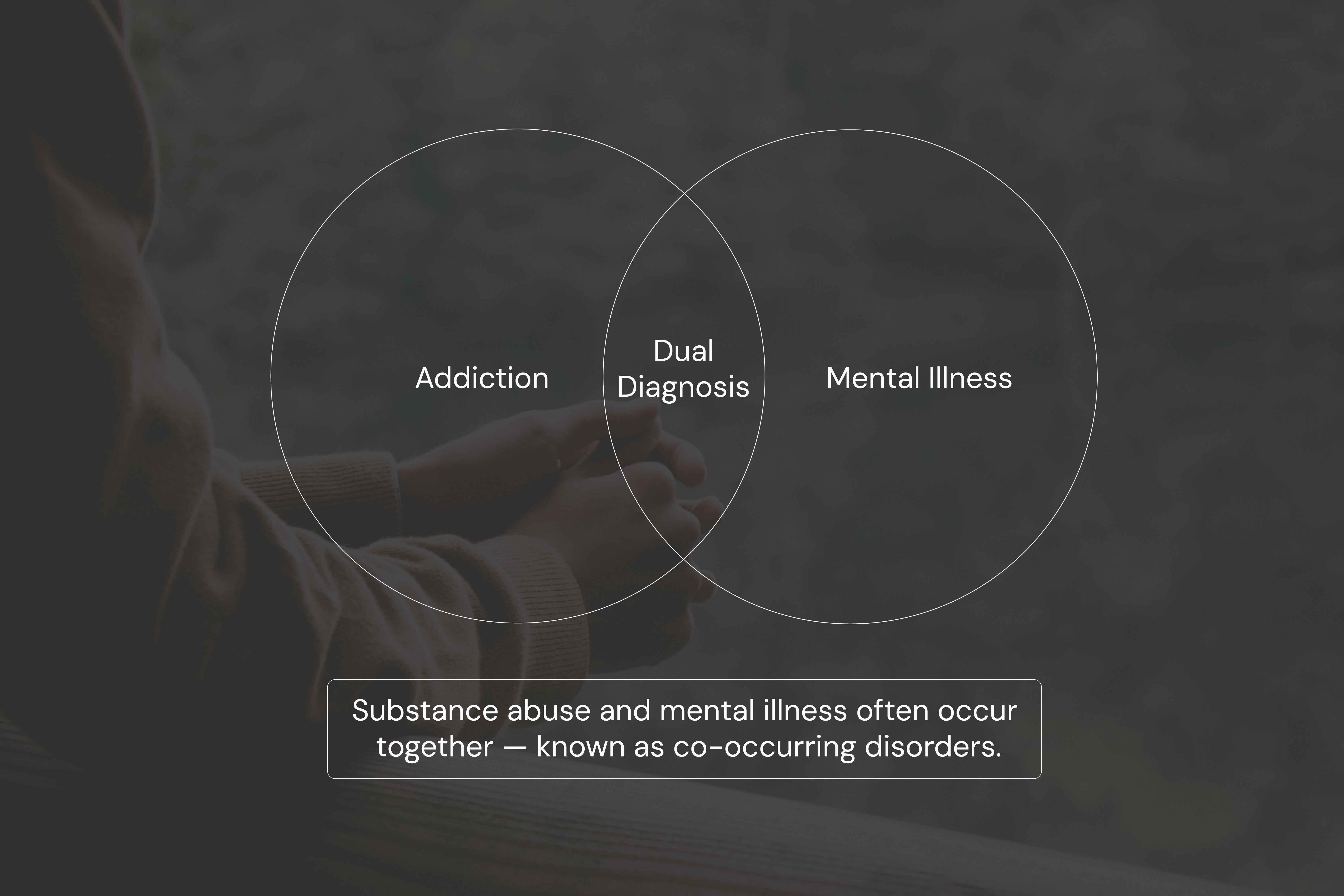
Substance abuse is classified as a mental health disorder and is often deeply connected to other psychiatric conditions. When both a substance use disorder and a mental illness are present, the diagnosis is known as a co-occurring disorder or dual diagnosis.
Understanding how these conditions overlap is key to effective treatment and long-term recovery.
What Is a Substance Use Disorder?
A substance use disorder (SUD) is a condition where a person loses control over their use of drugs or alcohol despite negative consequences. It affects behavior, brain chemistry, and emotional regulation, making daily life more difficult.
Common types of SUDs include:
- Alcohol use disorder
- Opioid use disorder
- Cocaine addiction
- Cannabis dependence
- Prescription drug misuse
SUDs are officially recognized in the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders) and are treated as legitimate mental health conditions.
Is Substance Abuse a Mental Illness?
Yes. Substance use disorders are classified as mental illnesses by the American Psychiatric Association and the World Health Organization.
There are three key reasons:
- They change how the brain functions over time.
- They involve psychological and behavioral symptoms such as cravings, anxiety, depression, and paranoia.
- They meet strict diagnostic criteria for mental health disorders.
In treatment settings, substance abuse is viewed as both a physical and psychological issue requiring comprehensive care.
What Are Co-Occurring Disorders?
A co-occurring disorder happens when someone experiences both a substance use disorder and another mental health condition at the same time. For example:
- Depression and alcohol misuse
- PTSD and cannabis use
- Bipolar disorder and stimulant addiction
These combinations can complicate treatment because each condition can amplify the symptoms of the other. In many cases, one condition may go undiagnosed if the other takes priority in care.
Why Do They Happen Together?
There are three major reasons substance abuse and mental illness co-occur:
- Shared risk factors: Genetics, trauma, environmental stress, and brain chemistry may all contribute to the development of both.
- Self-medication: Individuals may use substances like alcohol or benzodiazepines to reduce symptoms of anxiety or depression.
- Substance-induced symptoms: Long-term drug use can trigger or worsen psychiatric conditions. For example, stimulant abuse may induce paranoia or anxiety.
Recognizing the Signs of Both Conditions
Some signs that a person may be dealing with both a mental illness and a substance use issue include:
- Using alcohol or drugs to manage emotions
- Ongoing depression or anxiety despite substance use
- Withdrawing from family and responsibilities
- Difficulty focusing or completing tasks
- Experiencing cravings, withdrawal symptoms, or tolerance
Proper diagnosis requires a professional evaluation to determine whether the symptoms are caused by a mental illness, a substance, or both.
How Are Co-Occurring Disorders Treated?
These conditions are best treated together, not separately. Addressing only the addiction or only the mental illness increases the risk of relapse and incomplete recovery.
Treatment typically includes:
- Integrated therapy that addresses both disorders in tandem
- Medication for mental health symptoms and withdrawal management
- Behavioral therapies like CBT (Cognitive Behavioral Therapy) or DBT (Dialectical Behavior Therapy)
- Support groups or peer counseling to build long-term accountability and emotional stability
For long-term success, it’s important to access professional help that treats both aspects together. Many programs offer support that focuses on both substance use and the mental health factors driving it. In these cases, people often see the most progress when they enter into a treatment plan that includes both psychotherapy and structured recovery—this kind of integrated approach has been shown to be especially effective in co occurring disorder treatment and long-term recovery.

Examples of Common Combinations
Some common co-occurring conditions seen in treatment centers include:
- Alcohol use and depression: Alcohol is a depressant and can deepen existing mood disorders.
- Benzodiazepine misuse and anxiety: Short-term relief can lead to long-term dependency.
- Cannabis use and PTSD: While cannabis may dull trauma symptoms, it can also reduce motivation and intensify emotional instability.
- Stimulant abuse and bipolar disorder: Stimulants can trigger manic or depressive episodes, complicating mood regulation.
- Nicotine or alcohol use and schizophrenia: These substances are frequently used in an attempt to manage cognitive or emotional symptoms.
Each pairing requires customized care to prevent relapse and support mental health recovery.
Challenges in Diagnosis
Because symptoms of substance use and mental illness often overlap, diagnosis can be difficult. For example:
- A person in withdrawal from alcohol might appear anxious or depressed.
- Stimulant use can cause symptoms that mimic psychotic disorders.
That’s why a thorough psychiatric evaluation is needed to separate substance-related effects from standalone mental health issues.
Why Early Detection Is Critical
Getting help early can significantly reduce the severity and duration of both disorders**.** Without treatment, co-occurring conditions can lead to:
- Higher suicide risk
- Homelessness or job loss
- Incarceration
- Emergency hospital visits
But when addressed together through coordinated care, people can achieve stable recovery and better quality of life.
How Substance Abuse Affects Mental Health
Substance abuse doesn’t just co-exist with mental illness, it often makes it worse. Drugs and alcohol alter brain chemistry, which can trigger anxiety, paranoia, or suicidal thoughts. People with pre-existing mental health conditions may find their symptoms magnified by substance use.
Understanding this connection is key to building a recovery plan that works. For more on how substance use worsens psychiatric symptoms, check out How does substance abuse affect mental health.
Conclusion
Substance abuse is a mental health disorder. It affects how the brain functions and behaves, and it frequently co-occurs with other psychiatric illnesses. When these conditions overlap, the best approach is integrated care that treats both simultaneously.
Recovery is possible, and it starts with acknowledging the link between mental health and substance use, and finding support that addresses both together.







